Care has a hefty history... but can it get over all that and change its narrative to hope?
When it comes to elder care and the disastrous culture around it - explanations are certainly needed. The past, they say, can help explain our present.
Despite aging being a source of fascination for thousands of years, ‘Care for older people’ only became a conscious ‘idea’ in the 20th Century. [1]
Previous to this the obsession was pseudo medical; seductive, vague snake oil ideas to increase one’s life span, or the promise of life after death. Such approaches were also mixed with a blame culture, judgmental and religious. A focus on atoning for the sins that result in sickness; our problem is who we are and our correction is to take place within the religious institutions. Here also we can find the idea of the carer as ‘holy’, ‘saintly’ endlessly ‘sacrificing’ for the benefit of others and the purification/negation of the self. [2]
In truth, we have not outgrown any of this childlike fantasy, and our culture very much still clings to fad diets, ‘potions’ for ‘health’ and all the trappings of blame around those that become unhealthy, or heaven forbid, fatter than the stick thin. We also continue to idolise the ‘caregiver’ while forcing them to work in the most terrible conditions. Aren’t they the modern day saint - the superhero - Endlessly sacrificing, despite themselves? They are ‘heroes’ aren’t they?! An unreasonable ask, of which we as a society should not be proud and is proving wholly unsustainable.
We must admit that the pace of human development around aging and care for older people is very… …very slow. The idea of caring for older people in a near civilized manner has taken thousands of years to get to. (the myth that people used to be cared for well at home, by the way, is just that, it’s a myth - a convenient lie told by people who have not lived through it) [3] care at home is rarely the best or healthiest route long term: [4] “They felt listless and tired, had a short temper, were often in a bad mood and the combination cost them a lot of energy. Some caregivers said that their life was no fun anymore and that the situation was overwhelming them. They experienced burn-out symptoms or physical complaints such as shortness of breath, tiredness, a need for antidepressants, panic attacks, headaches or crying episodes” “Japan, have explicitly moved away from this because of the recognised deficiencies of family care, such as the pressures it places on informal carers.”[3]
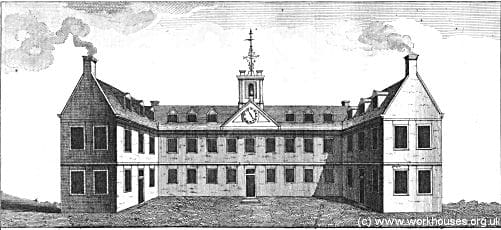
[1] Up until the 1500’s care in the UK was dispensed by the religious orders. However after the dissolution of the Monasteries increasingly the guilds and wealthy benefactors began to take over. The Poor Laws started to be continually updated and Work Houses began to appear alongside the almshouse. The idea of the ‘worthy’ poor being cared for more humanely, and for the ‘unworthy’ going to the Workhouse became standard. [5]
I would suggest that we watch for these trends in our approach to modern care, with lavish ‘extra care’ and retirement facilities for those that in fact remain very, or relatively able as they age, and deeply problematic nursing homes for everyone else.[6]
We all like to think we will be the healthy one - however the reality is that somewhat over 1 in 3 of us will need to use a nursing home at some point as we get older [7]. Instead of running from the issues, we need to start taking them seriously.
[8] Workhouses “designed to deal with the issue of pauperism, in fact became prison systems detaining the most vulnerable in society.”. [9]
(and all too often the ‘prison’ mentality remains all to close to the surface, especially when the building plans are too similar to that of prisons and our political leaders suggest older people can be cared for in the same way we care for our children… [3]…It is simply not right, and not possible, for us to wield the same level of control over adults as we do our children, or to draw any similarity between the two types of care)
By the early 1800’s
[10] “The Act recognised four types of inmate: the aged and totally ‘impotent’ (i.e. destitute through no fault of their own); children; able-bodied females; and able-bodied males. Accommodation was supposed to vary according to the individual requirements of these groups but since it was difficult to predict numbers, many workhouses opted for ‘general mixed’ accommodation.”
[6] As the 1800s progressed hospitals and rational medical science began to become more prevalent - with them, the modern problem of ‘bed blocking’ began. As Chronic patients could not be discharged due to their ongoing conditions and, as we still see today, “patients who were admitted for an acute problem but then were too debilitated to return home”.
Therefore, in the UK, hospitals at that time simply refused anyone who might pose a bedblocking risk: [1] “(hospitals) had a high reputation for good nursing and medical staff but did not admit chronic sick patients for fear of bed blocking. Consequently, medical students never saw them and were not taught about the diseases of old age. Workhouses were grim buildings, which discouraged admission. Their infirmaries had to accept patients refused by the voluntary hospitals and gradually become long-stay institutions for the chronic sick.”
But increasing social outrage at the quality of care and living conditions offered by both Almshouses and Workhouses, coupled with new waves of the government social reforms meant the beginning of the American style rest-home / Old Age Home in the UK:
“The 1905 Minority Report of the Royal Commission on the Poor Law advocated a need ‘to break up the present unscientific category of the aged and infirm’ and ‘to deal separately with distinct classes according to the age and mental and physical characteristics of the individuals concerned’. The 1941-1945 surveys of hospitals in England and Wales were equally frank, leading the Nuffield Provincial Hospitals Trust in 1946 to recommend a complete review of care of the chronic sick.
By the early 20th century care of an older relative was regarded as the concern of the State. Relatives came to view admission of an older relation to a chronic sick bed as ‘a bed for life’, and the patient’s home was given up…”
[11] Furthermore in 1908 the first pensions were brought into effect for anyone over the age of 70.
As the 1900’s progresses we see the beginning of regulations. They bring with them the first major wave of medicalisation of the care-home, and the creation of the nursing home, the change from person to perpetual patient and ideological turning of everyday life into a regimen of ‘treatment’ and ‘therapy’.
“In 1927, parliament passed the Nursing Homes Registration Act… …These laws made it compulsory to register nursing homes so they could be inspected, and introduced penalties for those who failed to do so. Homes also now had to keep proper records of every patient.”
Finally the 1948 National Assistance Act abolishes the Old Poor Law, the NHS is formed in the UK making health, finally, a concern of universal suffrage and Local Authorities become responsible for assisting ill, disabled and older people with care. With that the modern age of care is ushered in. The UK and USA are now more or less running in tandem when it comes to care and nursing homes:
[6] “The full transformation to a medical model, however, would come in the 1950s when, for the first time, government regulations were drawn up to end the most egregious of the many abuses commonplace in rest homes”
With government responsibility and public money comes increasing inspection and control, Muriel Gillick Discusses:
“Public health officials, not surprisingly, recreated the environment with which they were well-acquainted, the general hospital, minus the machines and the medicine”
“I thought this was a major mistake; older people moved to such facilities in order to live despite their disabilities, not to get better and move on. To focus exclusively on what was wrong with them, rather than to support and encourage whatever was right with them, struck me as profoundly misguided.”
“Something was profoundly wrong with nursing homes: They weren’t homey. As Robert Butler, the founding father of modern geriatrics, wrote, “A long-term care institution should be homelike—not sterile, antiseptic, or reminiscent of a motel. It should be a lively place with many ties to the larger community.”
“why were nursing homes medical institutions, even though they didn’t provide a whole lot in the way of medical treatment? Why were they run by nurses?”
It took a couple of thousand years to change caregiving from religiously based to the brutal beginnings of a rational model in the 1500’s. It took 450 years for that rational model to move away from a dysfunctional and abusive everyday lifestyle into a medical approach with inspected standards and ultimately its very own typologies of problematic institutional abuse.
Enter Tom Kitwood, 40 years later, in 1990’s UK and the birth of the idea of Person Centred Care. Yes, it’s only been agreed in the last 30 years that people in receipt of long term care should be viewed as individual human beings, deserving of, and needing a positive sense of their own identity.

Why in the 90’s? And how the heck do we get from there to Maracuja Club???
What was so special about Thomas Kitwood? That meant he could push the change?
[12] “THOMAS KITWOOD was a pioneer in the field of dementia care. He developed innovative research projects and training courses, challenging the "old culture of care". His aim was to understand, as far as is possible, what care is like from the standpoint of the person with dementia.”
Interestingly care for older people and dementia were not at all in Tom’s past - his focus was initially on religion. Clearly a man interested in the broadest sense in ethics and the human experience. Publishing his first book ‘What Is Human?’ shortly before he left the church in the 1970’s to study psychology, social and educational science. It was only by a chance commission that he began working with older people.
[13] His specialism was a field called Depth Psychology which stems from traditional psycho-analysis and psychodynamic therapies. Such approaches to psychology suggest that there are other (psychological, historic, social…) drivers of ‘symptoms’ and ‘behaviours’, they do not simply result from the traditionally medical physical and micro biological causes.
The key here is that Kitwood was not coming at dementia and older people as a clinician, a nurse or doctor. He was someone with a compassionate interest in the whole human being, his background and work meant he had a focused interest in the relationship of the person to their physical and social environments.
Tom Kitwood’s work was made possible by development of the field of psychology from Freud onward - he was at the cutting edge of this thinking being developed for and applied to the care setting.
The result of this? The blindingly obvious. Yet that which we as humans seem to continually run from, to the point that science and people like Tom Kitwood have to shove it down our throats, (for reasons which we will go into in a separate article): “a "person-centred" approach, quite simply to "treat others in a way you yourself would like to be treated"".[14]
Dr Croucher, writing for New Zealand Dementia Foundation says:[15] “when the prevailing medicalised system of care that I am a part of is so far out to one end of a spectrum of disease-focus versus person-focus, strident voices are needed to wake us all up. Thank you, Tom! !”
This is the basis of person centred care. Kitwood also introduced what I would call the first ever actual ‘training’ for care givers that is reminiscent of the training of the first professional sports people - it’s called Dementia Care Mapping. A process of observation and reflection within the live care environment. With review to discuss and practice behaviours, their causes and outcomes with the goal of improving the care givers’ skills.
Yet, the result of all this has not been the outstanding breakthrough you might expect. The dichotomy of person centred v.s. medicalised and the struggle to care well for people is still continually referred to as a kind of war - the foot-soldiers and casualties of which are those carers freely referred to as ‘heroes’ on the ‘front-line’ - a mad state of affairs to be sure - what do we think we are doing as a culture, allowing the situation to continue as it does? The system is so medicalised, and lead by people with such a narrow mindset to human health that their continual, innocent, backsliding is freely acknowledged and taken only lightly “It is also an excellent place to come back to if, like me, you could do with a repeat blast from Kitwood’s clarion trumpet.
It won’t be a completely comfortable read, but it will charge you up again to re-enter the fray with renewed enthusiasm.”
The innocence with which care is treated by both medical and business professionals continues to create issues:
[16] “Brown Wilson says... “It was a rude awakening to those who thought they were getting involved in housing or hospitalities. This involves peoples' lives," she says. "Building it was one thing. Running it was something else. People began to understand that this was a business of care, and you needed the capacity to deal with that to be effective.””
“To date, the main strategy for wide-scale nursing home change is more state and federal regulations and reforms.
"Some regulation is excellent and important, but the issues involved in today's nursing homes are so profound that we cannot regulate ourselves out of them," Gillick says.”
So why haven’t Tom Kitwood’s reforms taken meaningful hold? I can tell you simply that the science was not yet evolved to the point where we could describe the causes of wellbeing, or the causes of stress. We could not therefore respectively make them available or remove them for both customers and staff. Nor was the science evolved enough to give us any detailed guidance on a repeatable, clear modus operandi for the staff. Therefore, with little scientific substance on which to base practical training guidance has remained observational, overly anecdotal, and much too woolly in its descriptions:
[17] “In the light of the multiple meanings attached to the term in both metaphysics and moral philosophy, personhood is a relatively unhelpful concept to act as the foundation for developing models and standards of care for people with dementia. Care, we suggest, should concentrate less on ambiguous and somewhat abstract terms such as personhood and focus instead on supporting people's existing capabilities, while minimising the harmful consequences of their incapacities.”
[18] Comfort, attachment, inclusion, identity, occupation, love, are things we can all subscribe to, yet give us little guidance on concrete actions, modus operandi or behaviours that will help us, or help us to help others, achieve an optimally healthy lifestyle that suits them. Also in terms of outcomes, the science, and scientific measures weren’t there to guide progress, or create reflective goals for improvement.
We can’t simply give someone their favourite food every day, we can’t play their favourite song 24/7, we cant rely on people choosing their own clothes to give them a fulsome sense of identity, and so forth. These things are better than nothing, but there was simply not the detail in science at that time to add fuel to Tom Kitwood’s breakaway thinking.
But a lot of science has been done between the 1990’s and now.
Maracuja Club is the child of Tom Kitwood and that science:
Positive Psychology
Neuro-Psychology
Neuro-Science
Orientation
Sensory need
Attachment Theory and dependence
Peri-personal space and body schema
Positively and negatively affective mood states
Proven causes of wellbeing and associated measures
Studies of different approaches to, and types of, activity
Proven stressors and their elimination
Identity development
Cognitive bias
Flow theory and accessibility
The increasing acceptability of complex models of wellbeing. Bio-Psych-Social models for example are now becoming more common.
Understanding of memory, short/functional and long term.
Growing acceptance that the built/physical environment substantially impacts behaviours, experiences, quality of life and ultimately health.
Many new complex model approaches to providing care and their outcomes, which have now been studied.
Cognition, cognitive load and working memory.
And so much more.
Tom Kitwood did not have all of this to develop a concrete model, and moreover he was trying to insert a new way of working into a broken building typology that pervasively encourages the opposite behavioural modes in staff and residents.
We have to stop wallowing around, bouncing between models of care that have been tried and failed over the last 100 years. The only risk left in the care industry is to keep doing the same thing and expecting different results.
In Maracuja Club we have developed the first fully evidence based, outcomes focused, concrete approach to care delivery. We can now guide the staff very much as sports coaches do, along the lines of agreed strategies and practicable skills that stem from the science of enhancing people’s wellbeing, inclusion, accessibility and reducing proven stressors.
We then place that expert team into a building that - to complete the sports analogy - is the perfect field in which to carry out this new evidence based support community. It makes the receipt and delivery of care so much easier. It removes the staff and resident from muggy, internalized, institutionalizing, stressful, anti social behaviour generating residential corridors. Instead the new building gives green views, easy garden access, fresh air, enhanced orientation, sensory choice. It is now all you could ever want in an engaging community, that collaborates to create the very best days and lifestyle possible.
Maracuja Club places everyone on equal footing, so the staff and customers can work together for the very best experiences possible. We will be running through the staff modus operandi and resultant building typology in further posts. For now, suffice to say, it has been a long road for care to get to this point, many hundreds of years of the evolution of human society and science. The only risk now, is to not take this next step forward.
If you would like to support Maracuja Club, please do add your name. We are forming a syndicate of private and institutional investors to bring the project forward - if that sounds like you and you are interested in being part of the change the industry is waiting for, please get in touch.
1. Denham, M. A Brief History of the Care of the Elderly. 2016 23 June 2016; Available from: https://www.bgs.org.uk/resources/a-brief-history-of-the-care-of-the-elderly.
2. Ball, P. The God quest: why humans long for immortality
We can’t stop craving eternity. 2015 30 July 2015; Available from: https://www.newstatesman.com/long-reads/2015/07/god-quest-why-humans-long-immortality.
3. Needham, C. Why family care isn’t always the best care for the elderly. 2017 February 13, 2017; Available from: https://theconversation.com/why-family-care-isnt-always-the-best-care-for-the-elderly-72808.
4. Bijnsdorp, F.M., Onwuteaka-Philipsen, B.D., Boot, C.R. et al., Combining paid work and family care for a patient at the end of life at home: insights from a qualitative study among caregivers in the Netherlands. BMC Palliat Care, 2021. 20.
5. Association, T.A. History of almshouses. Available from: https://www.almshouses.org/history-of-almshouses/.
6. GILLICK, M.R. The Evolution of the Nursing Home. 2018 May-June 2018; Volume 106, Number 3, Page 186:[Available from: https://www.americanscientist.org/article/the-evolution-of-the-nursing-home.
7. Benz, C. 40 Must-Know Statistics About Long-Term Care. 2012 Aug 9, 2012; Available from: https://www.morningstar.com/articles/564139/article.
8. Brain, J. The Victorian Workhouse. Available from: https://www.historic-uk.com/HistoryUK/HistoryofBritain/Victorian-Workhouse/.
9. BLAKEMORE, E. Poorhouses Were Designed to Punish People for Their Poverty
In a time before social services, society’s most vulnerable people were hidden away in brutal institutions. 2018 AUG 29, 2018; Available from: https://www.history.com/news/in-the-19th-century-the-last-place-you-wanted-to-go-was-the-poorhouse.
10. Rich, A. The Elderly and the Workhosue. 2015 08 Nov, 2015; Available from: https://www.bgs.org.uk/resources/the-elderly-and-the-workhouse.
11. Munson, S. A History of Care Homes. 2020 7 Aug, 2020; Available from: https://www.carehome.co.uk/advice/a-history-of-care-homes.
12. Independent. Obituary: Professor Thomas Kitwood. 1999 6 July, 1999; Available from: https://www.independent.co.uk/arts-entertainment/obituary-professor-thomas-kitwood-1045269.html#comments-area.
13. Association, A.P. Depth Psychology. Available from: https://dictionary.apa.org/depth-psychology.
14. Rahman, S. Blame Alice: how language wilfully produces power imbalances in dementia. 2015 April 21, 2015; Available from: http://dementia-wellbeing.org/tag/kitwood.
15. Croucher, M. Person-centred care and Tom Kitwood’s legacy. 2020; Available from: https://www.nzdementia.org/Articles/blog-person-centred-care-and-tom-kitwoods-legacy.
16. Birnstengel, G. How’d We Get Here? The History of Nursing Homes. Caregiving 2021 March 5, 2021; Available from: https://www.nextavenue.org/history-of-nursing-homes/.
17. Gilleard, P.H.a.C., Interrogating personhood and dementia. National Library of Medicine, 2016.
18. Ley, P. The Flower of Emotional Needs. 2017 March 25, 2017; Available from: https://reflectionsgreenwich.com/2017/03/25/the-flower-of-emotional-needs/.
